Outcomes and risks of treatment
It should always be our duty of care to optimize outcome with the least possible intervention.
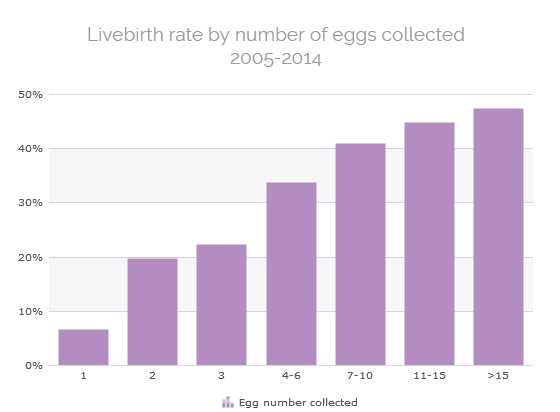
As you can see from the Livebirth Rate table of our data for the last 10 years (2005-2014), IVF success rate improves with increasing egg numbers collected, but there comes a point where the risks of ovarian hyperstimulation (OHSS, over-response that is one of the main complications of fertility treatments) increase without any real benefit in success rates.
Therefore we aim to optimize the balance between outcomes and risks of treatment.
Every Egg Counts
Even an increase from 1 egg collected (the likely maximum in a natural cycle) to 2 or 3 eggs significantly improves chances.
The table below shows the increase in livebirth rate from egg collection in all ages as we move from 1 to 2-3 eggs collected (Lister Fertility Clinic data 2006-2015).
| Aged <35 | Aged 35-39 | Aged >=40 | ||||
| Eggs Collected | No of Cycles | LBR / VEC | No of Cycles | LBR / VEC | No of Cycles | LBR / VEC |
| 1 | 72 | 8.3% | 238 | 5.9% | 538 | 2.4% |
| 2 | 111 | 18.9% | 408 | 12.7% | 732 | 6.7% |
| 3 | 161 | 23.6% | 503 | 18.1% | 784 | 7.0% |
How may Natural IVF harm my chances?
In those with regular cycles, the ovary produces one egg per month. Natural cycle IVF is a treatment cycle where the aim is to collect this single egg without the stimulating drugs given in a conventional IVF cycle.
The main risk of natural IVF is the cancellation rate due to no embryo being available for transfer from a solitary egg or premature ovulation. The latter can be minimized by using a “modified” natural approach. In such a “modified” natural cycle, no stimulation is used to encourage more follicles to grow, but just before collection medication is given to stop the single follicle from being released and to ensure it continues to grow.
Some clinics may push you towards “Natural Cycle” suggesting it to be the best treatment for you but there are some key facts you need to be aware of:
- 44% of Natural Cycles DO NOT result in eggs being collected
- 57% of Natural cycles DO NOT result in embryos being transferred
- The overall livebirth rate for Natural IVF is <5%
- It takes almost 5 natural cycles for every 1 stimulated cycle to achieve a livebirth.
- There is no difference in later pregnancy risks such as preterm delivery or low birthweight.
When might Natural IVF NOT be right for you?
Our ethos is to give every couple the best possible chance of success regardless of how that may affect our success rates.
If we think you have the ability to produce more than one egg if stimulated appropriately, then we will be likely to recommend against natural IVF.
At all age groups, even a small increase to 2-3 eggs significantly increases your chance of treatment success.
IVF success rates that are published as primary outcomes by the HFEA and do not include natural cycles. So, if you recommend those with a slightly lower egg number (and therefore lower chance of success) natural cycle IVF this may artificially keep clinic success rates raised by keeping these couples out of the official published data.
When is Natural IVF right for you?
In general, the doctors at The Lister Fertility Clinic advise patients to undergo a stimulated cycle because the success rates for IVF treatment improve with increasing numbers of eggs collected.
However, in those who are naturally ovulating and medication is unlikely to help recruit more than this one egg, “natural IVF” may be most appropriate. This is particularly the case in those with a very low ovarian reserve or in those who have previously used high doses of medication but still only achieved a single follicle.
As with mild IVF it may also be offered to those who have concerns over the side effects of medication, a medical problem where stimulation may not be possible or to absolutely eliminate OHSS risk.
Mild IVF
Mild stimulation IVF is one of the many tools at our disposal to minimize risk and is, in essence, just the sensible choice of a lower starting dose in a protocol that minimises hyperstimulation risk.
So, in patients with a good ovarian reserve and a higher likelihood of producing a good number of eggs, there is no benefit of using high doses of stimulation drugs. It is particularly suitable for women with polycystic ovarian syndrome who have a high risk of OHSS and in those with other medical conditions where risk of OHSS needs to be minimized.
Along with the use of mild IVF regimes, we also minimize OHSS risk by:
- optimising starting dose using a variety of ovarian reserve tests
- antral follicle count on scan
- measurement of antimullerian hormone (AMH)
- measurement of FSH levels
- endocrine monitoring throughout treatment with regular measurement of hormone levels to allow appropriate dose adjustments if needed.
- the use of alternative “ agonist trigger” injection where needed to mature eggs before collection that can virtually eliminate OHSS risk
- segmenting treatment cycles by freezing all embryos if necessary and transferring in a future natural cycle thereby allowing the body to recover and avoiding OHSS risk.
Mild regimes are therefore a vital tool in our armory, that are used in a significant proportion of cycles. Choice of protocol is always made after discussion of all relevant factors with our patients to help them decide whether to go for low, medium or high stimulation based on their condition and the risks of potential side effects.
 Ελληνικα
Ελληνικα  English
English